In 2015, malaria killed between 438,000 and 722,000 people, mostly in Africa, Asia and Latin America. On top of all that human suffering, malaria seriously hampers economic development in poor countries. The disease reduces overall labour productivity, reduces agricultural output, discourages investment and tourism, and damages educational outcomes due to high degrees of absenteeism among both students and teachers. Repeated bouts of malaria can also compromise the cognitive development of children.
The results are stark: researchers estimate that the economic costs of malaria range from 0.41 per cent of GDP in Ghana to a staggering 8.9 per cent in Chad. It is also estimated that if malaria and HIV were eradicated, foreign direct investment in the median sub-Saharan African country could rise by as much as a third, with all the potential for growth and economic opportunities that would entail.
The word “malaria” comes from the Italian words for bad (mal) and air (aria), for it was thought that the disease was caused by foul air emanating from swamps and bogs. In 1880, French army
physician Alphonse Laveran discovered that malaria was caused by a genus of parasites called Plasmodium.
Eighteen years later, British army physician Ronald Ross discovered that the malaria parasite was transmitted by mosquitoes. Soon thereafter, Italian zoologist Giovanni Batista Grassi identified Anopheles as the genus of mosquito responsible for spreading the disease. Once scientists understood the role of mosquitoes, they were able to develop programs aimed at halting the spread of the disease.
In the past, efforts largely consisted of spraying small amounts of the insecticide DDT on the inside walls of houses. Once sprayed inside, DDT repelled, irritated or killed mosquitoes. As Richard Tren of the public health advocacy group called Africa Fighting Malaria notes: “DDT’s public health applications were discovered by the Allied forces during World War II, and the United States was the primary backer of efforts to rid the globe of an ancient disease. After DDT fell out of favour due to somewhat overblown environmental concerns, new medicines and insecticides, and the use of insecticide-treated bed nets became more popular.”
Malaria is a stubborn disease, as mosquitoes tend to develop resistance to new insecticides relatively quickly, and widespread use of new tools, such as improved vaccines and genetically altered mosquitoes, are likely to be needed in the future. The sterile insect technique (SIT), for example, is an environmentally-friendly insect pest control method that involves the mass-rearing and radiation-induced sterilisation of mosquitoes.
The eunuchs are then released by air over defined areas, where they mate with wild females. The result is no offspring and a declining mosquito population. This method has already been successful in controlling a number of high-profile insect pests, including fruit flies, tsetse flies, screwworms and moths.
Environmental groups, including Friends of the Earth and the African Centre for Biodiversity, have raised concerns over the application of the SIT.
As Tren writes:
To be fair to those who oppose the genetic modification [of mosquitoes] there may be legitimate concerns, and it is right and proper to proceed with regulatory oversight … That said, there is little evidence that eliminating or dramatically reducing the populations of specific malarial mosquitoes would seriously affect other species that may rely on them as a food source. Another concern is that the technology could be hijacked by nefarious actors and even used to spread disease. While this is possible of course, it seems far from reasonable to block new technologies on the off chance that a rogue actor might attempt to hijack them. Were this the standard, would we ever have developed chemotherapies or radiation therapy for cancer treatments?
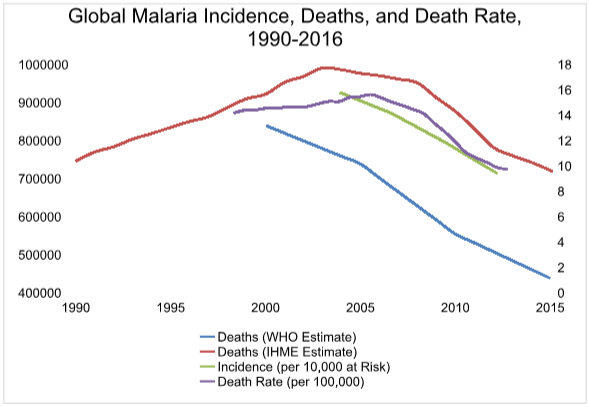
While there are hurdles to overcome, progress is certainly being made. Between 1990 and 2016, the malaria death rate dropped from 14.2 per 100,000 infections to 9.7 and incidence declined from 15.8 in 10,000 people in 2000 to 9.4 in 2015.
There is some debate among researchers as to the number of people who die from the disease each year. But according to the World Health Organisation, deaths from malaria declined from 840,000 in 2000 to 438,000 in 2015. The Institute for Health Metrics and Evaluation, in contrast, estimates that deaths from malaria declined from 746,000 in 1990 to 720,000 in 2016. Whichever statistics we choose it’s clear that while there have been great advances in the fight against malaria, much work still remains.